Source :NEWS18 NEWS
Last Updated:May 22, 2025, 16:26 IST
PCOS is a hormonal imbalance that can lead to frustrating symptoms like irregular periods, unwanted hair growth, acne, and sometimes challenges with conception.
Given the symptomatic overlap between PCOS and thyroid disorders — such as menstrual irregularities and ovarian cysts — thyroid function assessment is a critical step before confirming a PCOS diagnosis.
Ever feel like your body’s playing a confusing game with your hormones? If you’re experiencing symptoms like irregular periods, persistent acne, increased body hair growth, or difficulty conceiving, you could be dealing with a hormonal imbalance like Polycystic Ovary Syndrome (PCOS) and thyroid dysfunction, which are common partners-in-crime for many women. To get the correct diagnosis, it’s important to understand how these conditions are connected.
Dr. Pramila Kalra, HOD & Consultant, Department of Endocrinology, Ramaiah Memorial Hospital, shares all you need to know:
Recommended Stories
How PCOS and Thyroid Disorders Are Linked
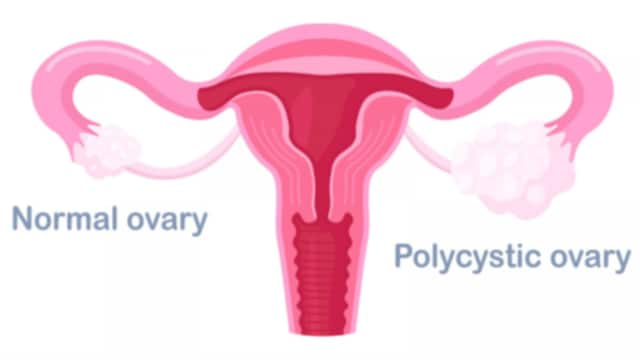
PCOS is a hormonal imbalance that can lead to frustrating symptoms like irregular periods, unwanted hair growth (often on the face or chest), acne, and sometimes challenges with conception.
Thyroid disorders, especially an underactive thyroid (hypothyroidism), are often caused by autoimmune conditions like Hashimoto’s thyroiditis — where antibodies attack the thyroid — a condition more common in women.
If you have PCOS, you’re significantly more likely to also have a thyroid issue. Sometimes, this thyroid issue can be subclinical, meaning it’s a mild impairment that may not present typical symptoms but still interferes with hormonal balance.
An underactive thyroid can throw off the hormones that regulate your ovaries. When your thyroid isn’t functioning properly, your body may produce more Thyroid-Stimulating Hormone (TSH) and another hormone called prolactin. This disrupts the delicate balance of Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH) — crucial players in your monthly cycle. When this balance is disturbed, ovulation can stop, and ovarian cysts (a hallmark of PCOS) may form or worsen.
Impact on Metabolism and Insulin Resistance
Insulin resistance — where the body’s cells don’t respond effectively to insulin — is a common feature of both PCOS and hypothyroidism. When both conditions coexist, the level of insulin resistance and dyslipidemia (such as elevated cholesterol) is often greater than in PCOS alone.
Thyroid hormone replacement therapy for hypothyroidism has been shown to improve insulin sensitivity and correct other metabolic disturbances in patients with concurrent PCOS.
If you’re juggling both PCOS and hypothyroidism, you may face a tougher battle with insulin resistance and notice higher cholesterol levels. Treating hypothyroidism with thyroid hormone replacement can help improve your body’s insulin response and ease other metabolic abnormalities.
Why a Thorough Check-Up Is Crucial
Given the symptomatic overlap between PCOS and thyroid disorders — such as menstrual irregularities and ovarian cysts — thyroid function assessment is a critical step before confirming a PCOS diagnosis.
Diagnostic investigations typically include blood hormone level analysis (including thyroid hormones), serum testosterone, DHEAS levels, and ultrasonography of the ovaries and thyroid gland. Accurate differentiation and diagnosis are essential to ensure women receive appropriate and targeted treatment for all coexisting conditions.
Before a PCOS diagnosis is confirmed, a thorough thyroid function check (usually a simple blood test) is essential. Additionally, evaluating other hormone levels is important to rule out disorders that may mimic PCOS.
- First Published:
May 22, 2025, 16:26 IST
SOURCE : NEWS 18